Recently, when a hygienist contracted a virus at work, it came on so quickly and aggressively that she ended up taking a whole month off at home to recover. Eventually, all of the other staff at her dental office, including front desk and clinicians, also came down with the same virus. After a month-long recovery, another hygienist described it as “the worst virus I had ever experienced”. She was concerned. The dentist office required that clinicians use personal protective equipment (PPE) such as masks, gloves, eye protection, and proper lab coats; however, they did not require a High Volume Evacuator (HVE) as a part of their safety protocol when working with powered instruments. Making matters worse, the vacuum pump lines were clogged with build-up that inhibited the air flow and limited the performance of the evacuation equipment at that office.
Illnesses are commonly shared in the workplace but the risk of exposure increases significantly for hygienists using powered instrumentation such as ultrasonic and air polishing . Bacteria and viruses can rapidly spread through splatter and aerosols produced by these types of treatments. The anecdote above given by the firsthand experience of one of the hygienists at the clinic described. While it can’t be proven that the viral infection was spread via contaminated aerosols resulting from powered instrumentation, it certainly offers a possible explanation for the office-wide epidemic. Powered instrumentation technologies have steadily increased to widespread use in North America ; however, safety standards and regulations concerning their use have not sufficiently evolved along with them. Only 24 out of 50 states in the U.S. claim they follow CDC infection control guidelines. While HVE is a top recommended solution for controlling aerosols and reducing the risk of contamination , many clinicians are still allowed to choose any suction device they prefer in order to perform their work. Saliva ejectors and isolation devices are a common choice even though they offer no safety protection from contaminated aerosols.
Dental healthcare professionals, educators and governments are faced with increasing urgency to change and improve health safety in dentistry. Some U.S. states and Canadian provinces have already mandated that HVE be used with all ultrasonic and air polishing procedures. Infection control guidelines, standards and regulations are currently under review by the Department of Health. We anticipate that these reviews will result in new, updated, and modified rule changes to include a mandate requiring the use of HVE across many more states. This needs to be a universal requirement and publicized with the same rigor as the anti-smoking campaigns that achieved bans on smoking in public places in the 1990’s.
WHAT IS HVE?
A High Volume Evacuator (HVE) is a suction device that draws a large volume of air over a period of time. This differs from a Low Volume Evacuator (LVE) which pulls a significantly lower volume of air. Air volume is measured in cubic feet per minute (CFM) and while both HVE and LVE maintain the same static vacuum pressure; the difference in air volume is due to the borehole size or number of holes in the evacuator tip. HVE devices typically have large, single bore or multiple openings, whereas LVE devices have a much smaller bore size. The standard HVE device commonly used in dentistry has a large opening and is attached to an evacuation system that will remove a volume of air up to 100 cubic feet per minute.
WHY DO WE NEED HVE?
Research shows that aerosols and splatter produced by ultrasonic and air polishing treatments contain saliva, blood, bacteria, and pathogens . Once airborne, aerosol particles can remain for an hour or more, lingering in the clinician’s breathing space and in the operatory, while splatter lands on the surfaces immediately surrounding the treatment area. This risks the spread of illnesses such as the common cold and influenza viruses, herpes viruses, pathogenic Streptococci or Staphylococci, the severe acute respiratory syndrome (SARS), and tuberculosis (TB).
While vaccinations for diseases such as the flu and H1N1 are available, neither the United States Centers for Disease Control and Prevention (CDC) nor the American Dental Association (ADA) mandate the use of these vaccines as a preventative safety measure. For illnesses such as TB or SARS, these agencies recommend that patients avoid elective dental procedures altogether, or have treatment done in a hospital. In Washington State, recent outbreaks of active TB have been reported by The Today file, and by the Washington Post. This is especially a concern with undiagnosed or undetected cases. A mandate for using HVE as a preventative safety measure is now more than ever, urgently needed.
HVE offers the best solution for controlling aerosolized particles before they leave the mouth. Studies have shown HVE to reduce over 90%-98% of aerosols regardless of source As there is no single solution that will provide complete protection, a combination of protective measures such as PPE, pre-procedural rinses, pre-polishing, and advanced air filtration systems, when used together with HVE offer the most effective and practical method of reducing the overall risk of infection.
HVE also offers better assurance against potential liability claims and a compromised public perception of the dental industry as a whole. From epidemics to fatalities, a single infection can lead to disastrous results. Until such a time when regulations and monitoring are implemented and enforced, the burden lies with individual dental teams to ensure that they are taking every measure necessary to maintain a safe and sanitary working environment.
HVE instruments have been shown to universally reduce airborne contamination, no matter what the dental source by 90% to 98%. Using an HVE is a mandatory infection control precaution during the use of an ultrasonic scaler. Harrel “Contaminated Dental Aerosols”
Evacuation devices on the market today vary by function according to the purpose for which they are designed. For ultrasonic scaling or air-polishing, the goal is not just water management; it is aerosol containment and controlling the risk of disease transmission. Saliva ejectors, isolation devices and standard HVE are among the most commonly used evacuation devices on the market today. Each of these has been studied for its effectiveness in reducing aerosols produced by powered instrumentation.
In a study by the ADA comparing HVE and a saliva ejector, results showed the HVE device to reduce up to 90% of particles reaching the clinician’s breathing space over the saliva ejector alone . The diameter of the saliva ejector is too small to be effective in removing aerosols and according to Stephen Harrel,“does not qualify as a high volume evacuator” . A JADA research report compared a saliva ejector to an isolation device for aerosol and splatter reduction during and after ultrasonic scaling. The findings of this study showed neither device to effectively reduce aerosols and splatter, nor was there a significant difference in the reduction of aerosols and splatter between the two devices . On the other hand, through his extensive research, Stephen Harrel concludes that a standard HVE tip removes 90-98% of aerosols regardless of the source and proves an effective solution to aerosol containment and reducing the risks of contamination.
While the results on the HVE studies are impressive, the conditions when operating in a clinical environment can be quite different from the test environment. In the field, hygienists must not only be able to efficiently use the device in the patient’s mouth but they also depend on the vacuum system and equipment provided at their dental clinic where age and other conditions may impact performance. They also need to work steadily in the patient’s mouth, ensuring their comfort, often while performing precision treatment with a powered instrument for a prolonged period of time. These are variables that may challenge the performance of an HVE device in ways that are not available in a test environment.
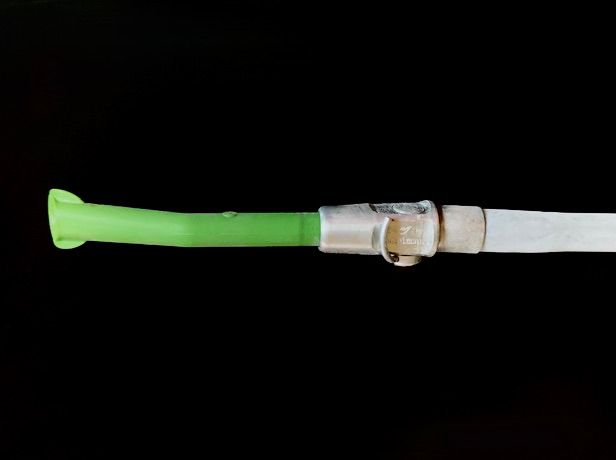
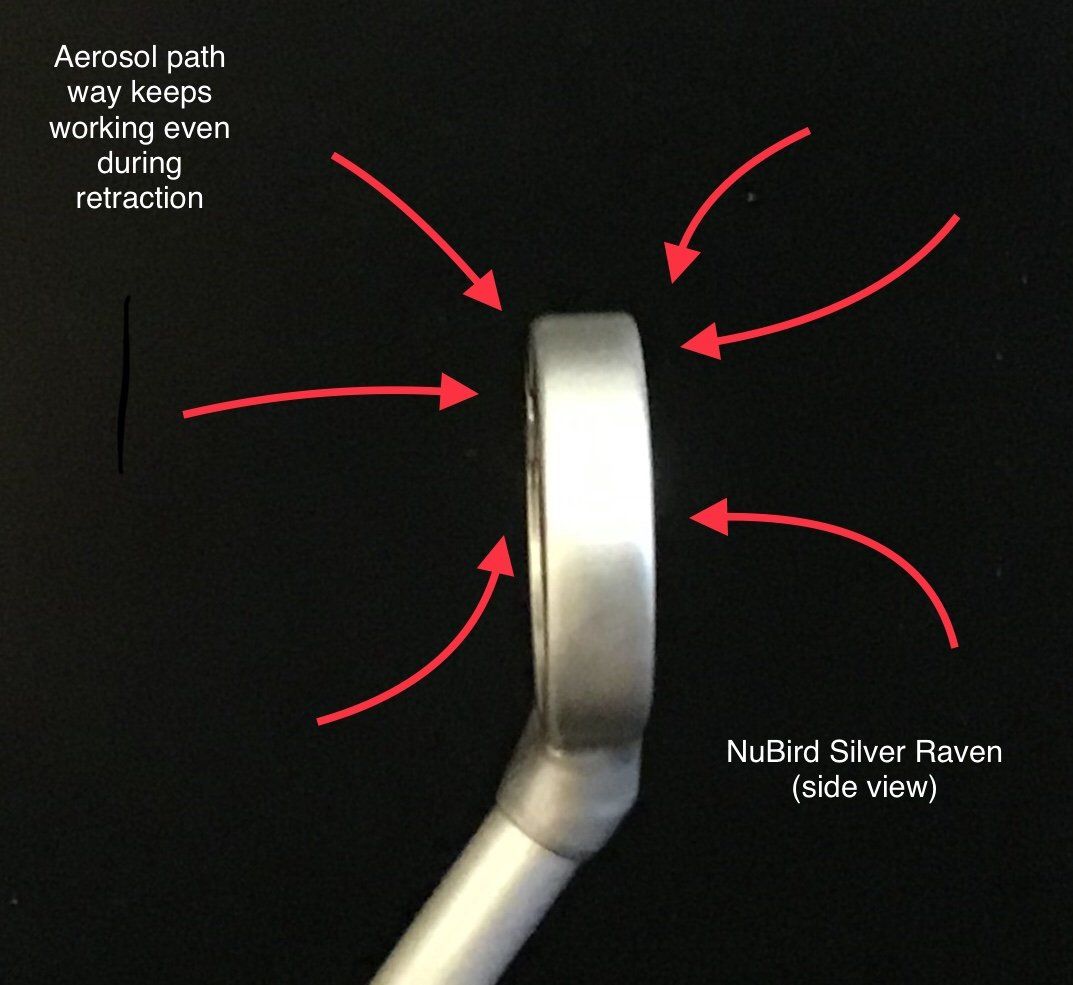
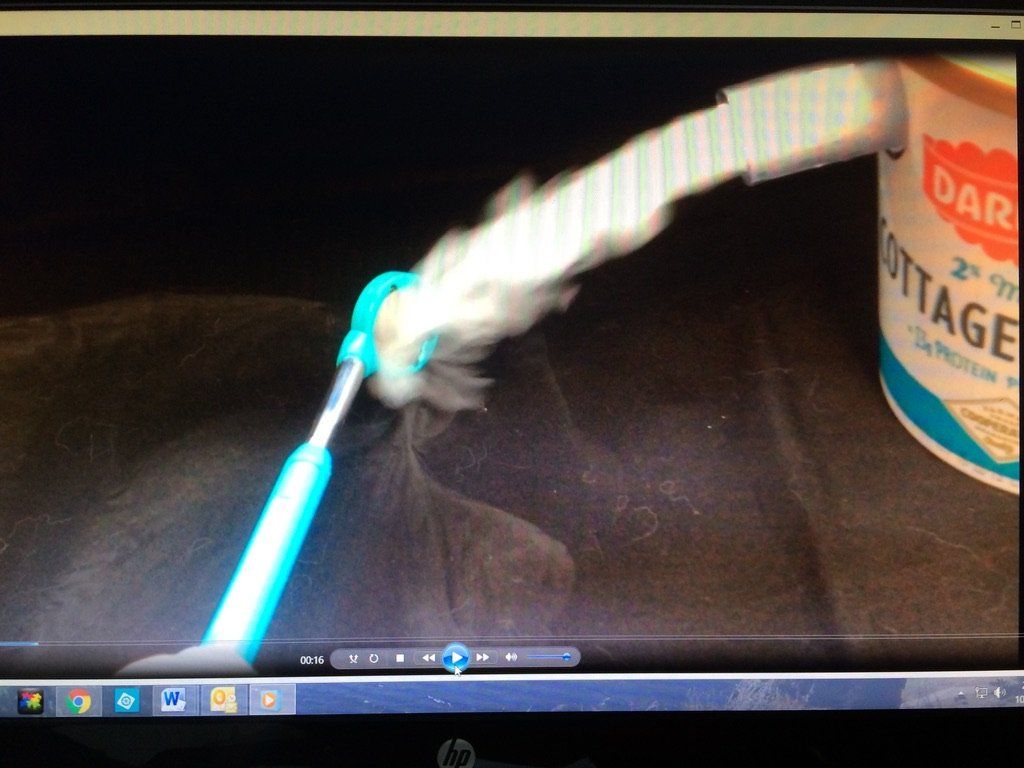
Above: Aerosol and water management using standard HVE tip and the new technology HVE Mirror System
HOW IS HVE MEASURED?
Vacuum gauges on evacuation equipment show the level of airflow (CFM) that was set by the manufacturer or service technician. The setting range depends on the size of the evacuation motor, the clinic, and how far the air has to travel from the motor to the user end; however, the only way to know whether an HVE device is working properly, is to test the volume of air flow coming out at the terminus or user end. Conditions such as age/strength of the equipment, build-up in the evacuation line, and number of users on the system can significantly impact the air flow at the user end; unfortunately, these variables are often overlooked. Currently there are no testing standards to measure airflow at the user end.
So how can we as clinicians tell if the power and volume of the HVE suction system are performing to adequate levels?
A simple timed water test is an easy way to test a device for suction performance at the user end:
TIMED WATER TEST
Start with a straight HVE tip and use a timer to measure how long it takes to pull up eight ounces of water. This will establish a control suction rate. Then measure the other devices against the control rate to gain an idea of how different devices compare against the standard HVE device.
SCIENTIFIC TESTS
To compare breadth of suction between instruments, we performed tests using both salt and equal amounts of sifted talc powder to simulate small particles and how different suction devices perform as they draw in the mediums.
In fig. 1 we placed salt evenly across a smooth flat surface. Using the straight tip HVE device, a saliva ejector (LVE), and an HV suction mirror to draw up the salt, we pulled each device through the salt at the same speed.
In fig. 2 we used talc powder with standard HV, saliva ejector, HV Suction Mirror and a saliva ejector adapted to HV. The results were impressive. Due to the wider footprint of the hole placement around the suction mirror head, the HV mirror was able to inhale a swath of particles that were two times wider than a straight tip HVE device.
THREE KEY CHALLENGES WITH USING HVE
As suction is often the secondary function to the dental procedure being performed, clinicians are more likely to choose a device which offers the greatest convenience and comfort so that they can more easily focus on their primary task. Since saliva ejectors are widely used as hand held and hands free, they are typically an easy option and first choice for managing pooling water. However, as studies have shown that they are not effective in reducing aerosols, saliva ejectors are a poor choice for use with powered instruments. While on the other hand, HVE is the best option, factors which can directly impact acceptance and clinical application of this technology include: performance, mobility, and ergonomics.
1. PerformanceClinicians need to know whether the power and airflow volume of their HVE suction system is performing to adequate safety levels. There are many devices on the market today that fit HVE ports but perform as LVE. As there is not standard safety measurement of air quality and vacuum performance, clinicians must rely on existing data from independent and manufacturer tests to determine the effectiveness of the devices they use.
As previously noted, vacuum performance can vary depending on the conditions of the system. A system can have clean lines and exhibit adequate airflow yet have extremely low static measurement of vacuum pressure (mmHg). This is where backflow could be experienced. In another example, an evacuation system might show a high static reading but have clogged lines resulting in low volume (CFM). When there are more users on the suction system loop, it tends to lower the volume and pressure. This may be experienced in larger offices. Most office suction systems have enough strength to remove pooling water but the lines can get clogged reducing suction volume performance.
[Just because an evacuation tip can be used on an HVE suction port to evacuate water and aerosols, does not mean it is operating at an acceptable suction level at the terminate or user end.]
2. Mobility
In order to work properly, HVE devices need to be hand held approximately 6mm-15mm away from the active ultrasonic tip or air polisher. For example, the device cannot be placed in the back of the mouth, like stationary devices, when the clinician works in the front of the mouth and vice-versa. Mobility is the key and there are at least a dozen locations within the mouth that clinicians need to access with HVE. The straight long shape of the standard HVE tip can be awkward to handle. Clinicians also need to pay careful attention to tip angulation to avoid getting the suction locked on their patient’s cheek or tongue. Ultimately, clinicians need to be able to move their suction device within their patient’s mouth without risking discomfort, all the while keeping focus on the treatment they are performing.
3. Ergonomics
Ergonomic limitations can make the clinician’s job more time-consuming, difficult to perform, or cause long term injury:
- A normal HVE hose weighs approximately one pound and feels very stiff to manage. Hygienists complain of too much pull on the wrist and arm, which can lead to repetitive strain injury.
- Because HVE devices are handheld, clinicians are unable to use their mouth mirror for indirect viewing. Reliance on direct vision only can cause excess strain on the neck by stretching over the patient to see what they are doing as they work.
- Due to limited visibility, clinicians typically have to take extra time to lay down the HVE device and check all areas with the mouth mirror and then rescale the spots they missed. Better functionality and efficiency is important for completing tasks within allotted time.
Ultimately, the question should be "which HVE system is most effective for aerosol reduction while maintaining clinician ergonomics, ease of use, and patient comfort?”
IS THERE A SOLUTION?
How do we address these problems and encourage hygienists to use HVE as a safety standard for all ultrasonic treatments?
In order to get hygienists to embrace HVE for safety and efficiency with powered instrumentation, the following concerns must be addressed:
DEVICE DESIGN: WHAT DO CLINICIANS NEED TO LOOK FOR?
New HVE devices are available on the market with practical features that offer innovative solutions to the ergonomic and mobility challenges of the standard straight tip model. Beginning with performance, clinicians need to look for devices that operate at higher velocity evacuation levels for reducing aerosols and splatter. From an ergonomics and mobility perspective, clinicians need to look for design elements that offer:
- Full mobility that is easy to handle in all areas of the mouth
- Broad sweep suction that inhibits the device from sucking up tissue
- Lightweight design that reduces the risk of injury
- Multifunctional capability that eliminates the need to switch devices mid-procedure
One example of an HVE solution that meets the criteria listed above is the HV Suction Mirror System by Nu-Bird Inc.
REGULATION STANDARDS, TESTING, AND CERTIFICATION
Currently, the health and safety of clinicians, office staff, dentists and their patients are too loosely guarded; tighter controls are needed. Dental health-care professionals must be made aware of the risks associated with aerosols and splatter produced by ultrasonic and other devices. With so much at risk, governments and the dental industry must take immediate action towards regulation and standards requiring the use of HVE as a preventative safety measure with powered instrumentation:
- Mandatory use of HVE during ultrasonic, laser, and air polishing procedures should be universally enforced.
- Measurements for air quality and safe suction levels must also be defined, benchmarked, and standardized.
- Clinicians also need to know if the power and airflow volume of the HVE suction system is performing to adequate safety levels chairside at the user end. In the same way that water lines and sterilization units are monitored at user end, evacuation air flow measurements should be so too.
- Dental office equipment should also be tested and certified to ensure that they perform as required for reducing aerosols and splatter. An annual user end vacuum airflow and static pressure certification program would ensure that these systems are performing effectively.
TRAINING
Today’s hygienists need to apply themselves to learn about and utilize new technology systems which can offer better HVE performance and improved ergonomic benefits. It is imperative that HVE be taught at the fundamental level in dental hygiene and dental schools, and enforced in general dental practice. Dental schools, manufacturers, and regulation enforcement agencies need to take steps to provide programs and material to advance clinical skills and compliance with upcoming changes in dental care safety.
CONCLUSION
It is vitally important for clinicians to utilize ultrasonic, air polishing and laser technologies and so positive steps have been taken to support the evolving health safety needs in dentistry. A few U.S. states and Canadian provinces have mandated the use of HVE with powered instrumentation . Dental hygiene schools have also taken steps to advance the clinical skills of their students in health and safety practices. However, there is still a road ahead for changes in industry regulations and standards for the health and safety of dental health-care professionals and their patients. Programs for testing, monitoring and maintaining performance of vacuum systems in dental offices and HVE devices at the user end are still needed. The time is now to take necessary steps to do better to manage aerosols for preventing the spread of disease in dental offices and to provide a safe and healthy environment for us all.
Article By Laura Emmons, Cheri Wu and Tia Shutter